This guide has everything you need to know about how the diaphragm and pelvic floor may impact your patient’s movement and symptoms in the real world.
So if you want to:
- Look at the body as a whole without getting overwhelmed
- Understand how the diaphragm and pelvic floor can impact the shoulder and hip joints (and symptoms around these areas)
- Increase clarity on the interaction between the diaphragm and core muscles
- Make sense of your patient’s assessment findings when they are highly stressed
- Implement a simple approach to the diaphragm and pelvic floor that gets lasting results
Then keep reading…
Contents
- Functional Anatomy Of The Diaphragm And Pelvic Floor
- Little Known Kinetic Chain Reactions To The Diaphragm And Pelvic Floor Floor
- The Role Of Stress On The Musculoskeletal System
- Putting It All Together With Easy Diaphragm And Pelvic Floor Muscle Training Exercises
Functional Anatomy Of The Diaphragm And Pelvic Floor
In this chapter, I’ll take you through the key anatomy you need to know about the diaphragm and pelvic floor.
I’ll also show you why it’s important to understand the functional anatomy of the diaphragm and pelvic floor so you can make sense of your patient’s objective assessment findings without getting confused.
Let’s get started.
Basic Anatomy Of The Diaphragm And Pelvic Floor Muscles
First, let’s get the basic anatomy lesson out of the way…
“The diaphragm is a thin skeletal muscle that sits at the base of the chest and separates the abdomen from the chest…” – www.healthline.com
“The pelvic floor muscle or pelvic diaphragm is composed of muscle fibre of the levator ani, the coccygeus muscle, and associated connective tissue which span the area underneath the pelvis.” – www.wikipedia.org
Real-World Implications Of The Anatomy Of The Diaphragm And Pelvic Floor
To cut straight to the chase…
Contained in the abdomen, the diaphragm muscle attaches to the ribcage and hence can influence rib cage movement.
The pelvic floor muscles attach to the pelvis and hence can influence pelvic movement.
This can work the other way round too… move the ribs and pelvis, you’ll influence the diaphragm and pelvic floor muscle function.
Breathing Muscle
The diaphragm is a primary breathing muscle and a device that exerts control over the lungs. It will shorten and flatten downwards when we inhale… which will elevate, anteriorly translate, and externally rotate the ribs… (unless you consciously block these movements).
The pelvic floor will lengthen when we inhale… and travel downwards as the pelvis moves towards anterior tilt.

Notice the diaphragm flattening… as the transverse abdominis and rectus abdominis expand
The diaphragm muscle will travel upwards as you exhale… and the ribcage will depress, retract, internally rotate.

Notice the diaphragm lengthening… as the transverse abdominis and rectus abdominis shorten and the pelvic floor muscles contract.
When exhaling, the pelvic floor muscles will return to the original position upwards… while the pelvis will go towards a posterior pelvic tilt.
Working together… on inhalation the diaphragm shortens and travels downwards… the pelvic floor muscles also need to travel down and lengthen… to allow your organs the opportunity to mobilise.
When you exhale… the pelvic floor muscles travel upwards and shorten… while the diaphragm lengthens into a dome-shaped muscle… and the organs will again move together.
For simplicity in this article, I’ll focus more on the diaphragm movement… you just need to understand that they rely on each other… the pelvic floor muscles doing the opposite contraction type… but moving in the same direction.
The diaphragm and pelvic floor are also more commonly recognised for their roles as core muscles and working as part of a team offering core stability,
aiding posture, and supporting the spine.
Little Known Kinetic Chain Reactions To The Diaphragm And Pelvic Floor
Now, before we get into real-world applications…(if you don’t know much about me yet, you’ll soon learn ALL my teaching, content and the information I share is not designed to sound smart and overwhelm you but keep things simple so you can have clarity and apply it in the real world)…
I want you to understand that the diaphragm and pelvic floor DOES NOT CAUSE all of the issues below…
These are just reactions.
These are not magic bullets that will solve all of your problems…
But they are very important muscular tissues to consider…
…and probably will need to be addressed as part of a holistic treatment approach… that looks at the whole person and not just the site of pain.
With that said, let’s dive in…
The Vital Link In The Human Body Between The Abdominal Muscles, Pelvic Floor And Diaphragm
Here is some important information to consider in your everyday practice for musculoskeletal or sports injuries:
The transverse abdominis will lengthen or eccentrically contract whilst inhaling and will shorten naturally when exhaling…
Or said another way… the transverse abdominis will naturally contract and ‘hollow’, ‘suck in’… when the diaphragm lengthens.
The obliques and rectus abdominis abdominal muscles will contract concentrically when the diaphragm lengthens… as this allows your ribcage to depress under the dome it forms… while the obliques depress and retract the rib cage.
How A Physiotherapist Can Use This Knowledge In Their Assessments
Think about touching your toes and the need for ribcage depression and retraction. The internal obliques are very important for this movement… They need the diaphragm to lengthen to do their job well…

Notice the lack of ribcage depression and retraction… when this patient touches their toes. Although exaggerated for teaching purposes… a lot of back pain patients will use this type of strategy.
Can you see how this is starting to fit together?
If Not, Don’t Stress..
Click here to download the expanded PDF version of this article with clinical examples, and then keep an eye out for an email from me in the coming days. I’m going to walk you through a video of how all this works in an assessment with a patient.
A common activity that your back pain patients may often struggle with first thing in the morning… is putting their socks on.
This requires almost maximal ribcage depression and retraction… and hip flexion and posterior pelvic tilt… which will require the diaphragm and pelvic floor to mobilise… towards the end of their natural ranges.

Putting on your socks requires the diaphragm to be able to lengthen fully… along with the pelvic floor to ascend.
The glute max will contribute to posteriorly tilting the pelvis… which may be a muscle you target a lot or a pelvic motion you use in your treatment plans? Or said another way… your patient requires the pelvic floor to mobilize, ascend or shorten… to aid their posterior pelvic tilt.
Taking this one step further… you would ideally like the diaphragm to lengthen and the pelvic floor to shorten… to help the glute max and transverse abdominis to contract concentrically naturally… during many basic movements in everyday life.
The Role Of Stress On The Musculoskeletal System
The key most therapists forget is, if you want to get and keep positive long-lasting changes, you must learn to look at the person in front of you rather than just the site of pain.
You must learn to understand the person’s story… make sense of the objective assessment… explain the problem (not the symptoms or diagnosis but what is actually causing the symptoms, specific to their story)… and solution (a step by step graded exposure to load tolerance)… specific to their actual needs and wants in life… rather than just giving some generic exercise to every patient.
With that said, let’s start making sense of the patient’s story in front of you…
BE WARNED ABOUT USING COOKBOOK RECIPES AND DIAPHRAGM ‘HACKS’
When I first started looking at the body this way… I spent a lot of money on courses and experts that taught me exercises on how to build muscle strength, mobilise, reposition, hack, release the diaphragm… and get these quick ‘wow’ results…
Exercises that you basically followed EVERY TIME for EVERY PATIENT.
BUT BE WARNED… cookbook recipes combined with a little bit of information can be VERY VERY dangerous.
Approaches like this… WILL be found out quickly… in high-pressured environments such as a professional sport or private practice.
I learned that lesson the hard way and I don’t want you to make the same mistakes as me.
Now please don’t get me wrong, these courses have definitely influenced my thought process but I think there’s a smarter and more simple way to put it all together without getting too carried away…
So after trying all this stuff out… and getting ok results for some patients and actually flaring up others… I spent a lot of time, effort, and more money searching for answers.
And to cut a long story short, what I found is that it all comes down to the person in front of you.
You need to ask the BIGGEST QUESTION of all:
“Why did this person’s diaphragm and pelvic floor lose the ability to lengthen in the first place… specific to their story?”
Or you could ask the question another way…
“Why did this person’s ribcage and pelvis lose the ability to go through a full range of its normal physiological range of motion… specific to their story?”
As we mentioned at the beginning, the diaphragm and pelvic floor can influence the ribs and pelvis but the ribs and pelvis can also influence the diaphragm and pelvic floor.
Remember, every person’s story is different.
The diaphragm and pelvic reactions are actually REACTIONS to that person’s story.
Can you see now why these ‘cookbook’ recipes will only get you so far?
A Sensitised Respiratory System Affects The Diaphragms Ability To Lengthen
When you appreciate the impact of previous injuries or ‘stressors’ as I like to call them… and specifically in regards to the diaphragm and pelvic floor…
…periods of prolonged stress (think issues at home, work, traumatic events) non-physical ‘stressors’… can become important to understand in your subjective assessment.
Chronic emotional stress and increased mental load can alter how the respiratory system works… in several ways;
- Respiratory drive
- Breathing pattern and timing
- Metabolic appropriateness of the respiratory response
The increased respiratory drive is essentially.. evidence of the body’s readiness for action… and will more than likely be in ‘fight or flight’… or also known as the sympathetic division of the autonomic nervous system.
The problem with the increased respiratory drive (think of an extreme example, someone hyperventilating)… is that the person inhales very quickly (shortens the diaphragm)… but has a very short exhalation (not a lot of lengthening of the diaphragm happening).
This will then have an impact on #2… the breathing timing and pattern… where your brain just wants to keep you alive… and so will find a solution to this problem.
This is usually in the form of relying on the scalenes to do more work… along with the accessory respiratory muscles… such as the sternocleidomastoid, pec major, minor, serratus anterior, latissimus dorsi, and serratus posterior.
If you list these muscles that may have to do more work out below:
- Scalenes
- Sternocleidomastoid
- Pec Major
- Pec Minor
- Serratus Anterior
- Latissimus Dorsi
- Serratus Posterior Superior
You should notice that these muscles are very common muscles that you may be either trying to inhibit throughout therapy via hands-on treatment… or strengthen sometimes for the majority of shoulder and neck pain patients.
It’s worth noting and crediting Postural Restoration Institute and Ron Hruska with speaking about these ‘chains’ of muscles probably before I was even born. I personally don’t follow a particular chain approach or PRI methodology in everyday practice yet I still think it’s useful information to be aware of.

Hyper-arousal brought on by mental & emotional processes… contributes to allostatic load… and affects the capacity of the body to maintain its stability and response to change… (think chronic or frequently repeated stress without sufficient recovery).
The body’s physiological processes adapt to the demand… and this respiratory rate essentially becomes the norm.
The body will find a way to keep going.
Now here is where it gets really interesting…
…. and you start to see similar reactions that happen with people in pain through all the various systems… such as the musculoskeletal and respiratory systems.
The anticipation of coming physically and emotionally stressful events has a distinct effect of increased respiratory rate… reducing the time spent exhaling and changing the respiratory pattern.
Much like the ‘perceived threat’ of a painful experience that may or may not be actual damage… the respiratory system reacts just like the rest of the body… by becoming sensitised… and contributing to pushing that person further into ‘fight or flight’… increasing the respiratory rate along with the heart rate and blood pressure.
Increased heart rate and breathing rate will decrease heart rate and breathing variability.
And, just like movement variability… we ideally want to be able to access as much variability as possible when needed.
When your nervous and respiratory systems are responding to emotions rather than metabolic cues from chemoreceptors… it may not be aligned with the actual physical needs of the body or your metabolic requirements.
Think of anything that is stressing you out while sitting on the couch trying to read a book.
You feel the adrenaline kicking in…
Your heart rate increases…
You notice your breathing rate increases…
Your ability to focus on the book is limited…
You don’t comprehend what you are reading…
Is your body reacting appropriately (heart rate, adrenaline levels, breathing rate) to sitting on the couch reading a book?
All of these changes happen subconsciously via thoughts and the emotions corresponding to those feelings.
Now hopefully you can see that mental and emotional factors… such as fear, grief, anxiety or depression… may start to impact how your breathing is now becoming regulated…
Homeostatic and biomechanically inappropriate breathing is associated with the anticipation of action… that does not actually occur.
Think about your back or neck pain patient sitting at a desk in their office… and their boss who has been giving them a hard time of late starts walking towards them.
Your patient’s breathing rate and depth are completely inappropriate for the situation… and are in fact probably more appropriate for a lion bursting into the room, ready to attack them.
Just like you reading the book and thinking about something that’s ‘stressing you out’…
A completely inappropriate response to someone sat working at a desk all day.
Do you see how a patients environment all of a sudden becomes important in where they use your strategies?
Is All Stress Bad? And The Secret To Helping Our Patients Build Resilience…
While working, sure, some ‘fight or flight’ is good… it’s the ability to get back into the ‘rest and digest’ a.k.a have variability that is the key… and from my experience, a lot of my persistent pain patients struggle with this.
Interestingly, inhalation is associated with the sympathetic nervous system… where the diaphragm flattens and the heart rate increases… while exhalation is associated with the parasympathetic nervous system… where the diaphragm lengthens and the heart rate decreases.
In simple terms, exhaling, a.k.a lengthening the diaphragm is an indirect way that helps us get into rest and digest.
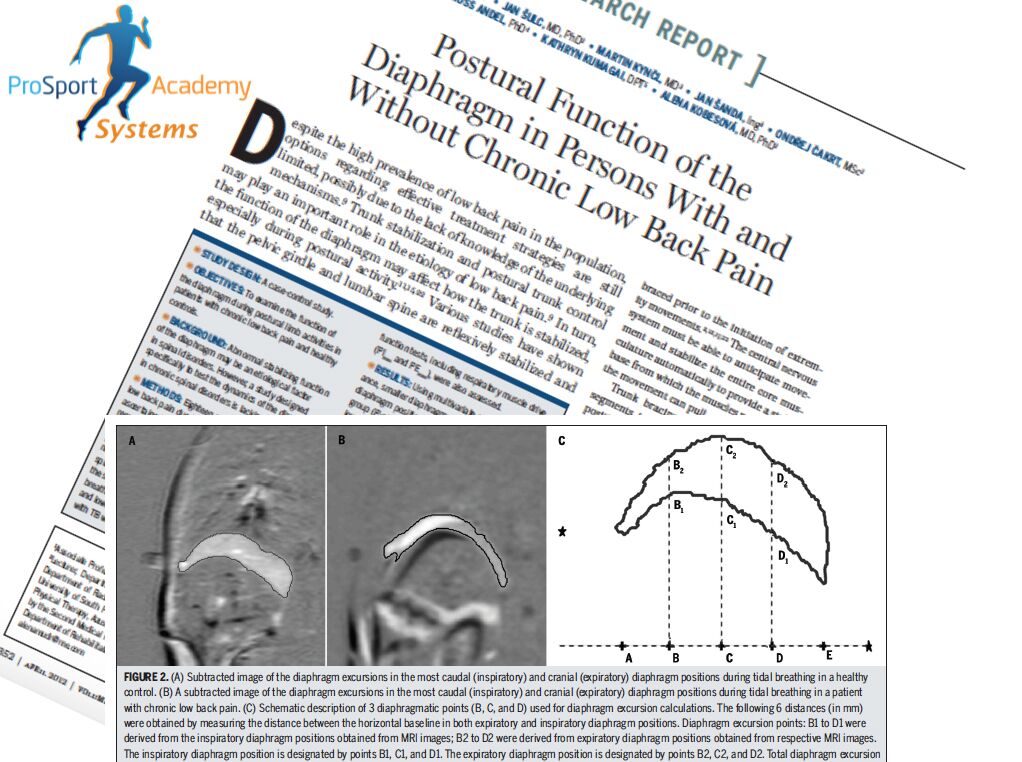
This study from a few years back shows the excursion of the diaphragm for people with and without back pain.
As we can see in the image below… notice the range of motion of the diaphragm… on the right-hand side of those patients without back pain versus those with.
Again… think about common strategies of your patients with back pain to bend over to pick an object up.
They will usually take a big breath, filling their lungs (shortening the diaphragm)… and move in a rigid motion with very little movement of the rib cage during the acute stage.
This further pushes your patient in a vicious circle of losing mobility through the diaphragm and ribcage… while further moving towards ‘fight or flight’.
In the short term it might be an ok strategy for acute pain experience, but in the long term what are the implications?
From clinical experience… desensitising the respiratory system and increasing the heart rate variability… (indirectly via the respiratory system)… can have a massive impact on a persistent pain patients’ ability to sleep in ‘rest and digest’… and wake up actually feeling refreshed along with decreased pain.
In fact, just restoring some variability with various respiratory desensitisation techniques… that we teach in module 1 of the ‘Go-To’ Therapist mentorship... can make a massive difference to your patient’s pain levels… without doing any hands-on treatment or rehab.
Putting It All Together With Easy Diaphragm And Pelvic Floor Muscle Training Exercises
Let’s finish today by looking at how to use all of this information in the real world…
How To Help The Diaphragm And Pelvic Floor Muscle In The Real World
Getting the pelvic floor and diaphragm to work together is actually pretty straight forward and just needs your patient to take a few breaths in a strategic way.
Pelvic floor muscle training can be as simple as prolonging the exhale which will prolong the pelvic floor muscle contraction.
This is an incredible pelvic floor exercise.
I’ve outlined here one of the easiest self-diaphragm release exercises (sorry I personally hate the term release) I know…
You may be surprised at how hard it is for some people to prolong their exhale and hence contract their pelvic floor muscles.
Remember it may not be muscle weakness but rather an inability of the diaphragm to lengthen.
An even better question may be ‘what is the patient’s true stressor that is causing this inability to prolong the exhalation?’
Concluding Thoughts
The diaphragm and pelvic floor are not some ‘magic bullets’ or ‘special muscles’.
They are however important to be aware of because they can influence the ribcage and pelvis and hence the peripheral joints.
They also react to non-physical stressors such as emotions and hence why it is critical that the ‘Go-To’ therapist always looks at the person first and pain second.
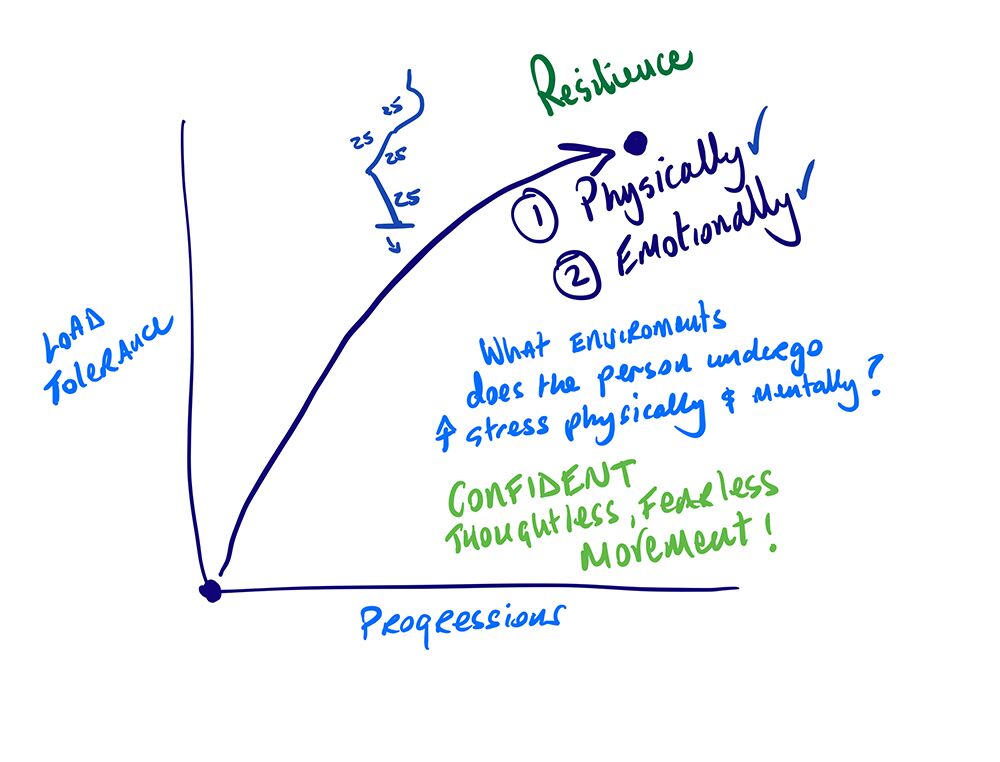
The first step is to undo these strategies and adaptations… and then most importantly increase the load tolerance specific to the person’s situation in a step-by-step graded exposure manner.
When you appreciate the reactions that can happen peripherally when the diaphragm and pelvic floor lose an ability to go through a full range of motion (which I’ll talk about in the next post), it allows you as a therapist an opportunity to work smarter, not harder.
Simple prolonged exhalation breathing exercises may undo some of these adaptations and allow the diaphragm an ability to go through an extended range of motion while slowing the inhalation will allow the pelvic floor to lengthen and the diaphragm to strengthen. Then you can continue to take the patient through a step by step graded exposure program without these muscles influencing other muscles at the ribcage and pelvis.
If you’d like this blog content in a PDF format to read later, and the videos of how to assess the diaphragm clinically in the real world, click on the link to download your copy now.
Now Over To You To Discuss The Diaphragm And Pelvic Floor Muscle…
So that’s my guide on the diaphragm and pelvic floor.
Now I want to turn it over to you: what did you think about this guide? Does the information help? Or maybe there’s something I missed.
Let me know by leaving any comments or questions in the special thread for this guide on the ‘Go-To’ Physio forums here.
Click Here To Join The Discussion Now



